Eye Library
Allergic Conjunctivitis

Amblyopia (Lazy Eye)
Amblyopia is the loss or lack of development of central vision in one eye unrelated to any eye health problem and is not correctable with lenses (eyeglasses or contacts). It is often associated with an eye turn (“cross eyed” or “wall eyed”), surgical complications, or a large difference in myopia, hyperopia or astigmatism between the two eyes. It often results from a failure to use both eyes together. Amblyopia usually develops before age 6 and is most often discovered during a comprehensive eye examination. Occasionally children will have symptoms such as noticeably favoring one eye or bumping into objects on one side. Early diagnosis of amblyopia is the key to increasing the chances of proper vision development. Treatment may include a combination of prescription lenses, prisms, eye patching and vision therapy.
Astigmatism
Vision condition in which objects at all distances appear blurry. Astigmatism may occur in addition to myopia, hyperopia or presbyopia. In this condition, light rays are split and not focused on the retina. This is due to the irregular shape of the cornea or crystalline lens inside the eye. Most often with astigmatism, the cornea does not have a perfectly round shape like a basketball but is more oval like a football. To correct astigmatism, eyeglasses or contact lenses are used to condense the light rays and focus them on the retina. Astigmatism is very common and most people have at least a small amount of astigmatism. Depending on the severity, patients may have no symptoms or may suffer from eyestrain, headaches and blurred vision. Contact lens options include soft toric, rigid gas permeable (RGP) and the new SynergEyes hybrid contact lens combining the sharp vision of an RGP lens with the comfort of a soft lens.
Blepharitis
An inflammation of the eyelids causing red, irritated, itchy eyelids. Blepharitis can masquerade as, and exacerbate, dry eye syndrome and allergic conjunctivitis. Blepharitis is classified into anterior and posterior. Anterior blepharitis is similar to dandruff with scales forming on the eyelashes. Posterior blepharitis is inflammation around the meibomian glands which secrete oils that help lubricate the ocular surface. The only way to properly diagnose blepharitis is by having our doctors examine your eyes under a medical microscope (a routine part of our comprehensive eye care). Blepharitis is very common alongside acne rosacea. Treatment depends on the specific type of blepharitis. The key to treatment is tackling the problem before it gets out of hand. Blepharitis seldom disappears completely and relapses are common.
We are excited to now offer BlephEX treatment to aid in the management of blepharitis. Click here to read more.
Cataract
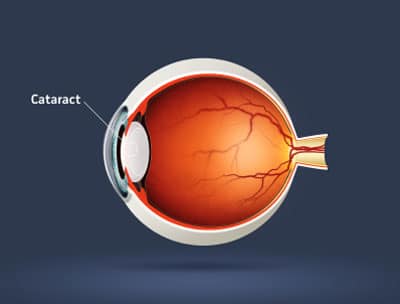
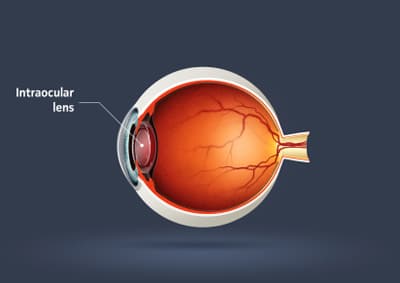
A cataract is a clouding of the normally clear crystalline lens within the eye. Our doctors evaluate each patient’s lenses during every comprehensive eye examination. Depending on size and location, a cataract may or may not result in decreased vision. Vision impairment from cataracts is typically slowly progressive over a period of months to years but may occur suddenly. Symptoms of cataracts include: blurred or hazy vision, increased difficulty in seeing at night, change in eyeglasses prescription, reduced perception of color intensity, and increased sensitivity to glare. Cataracts most commonly develop in patients over 50 years of age and can affect one or both eyes. Risk factors for cataracts include: advancing age, diabetes, some medications (including steroids), excessive ultraviolet (UV) light and eye injuries or surgeries. When a cataract interferes with daily activities, our doctors will evaluate your eyes for possible cataract extraction and intraocular lens (IOL) implantation surgery. We work closely with cataract surgery subspecialty ophthalmologists to ensure excellent results.
Chalazion
Inflammatory enlargement of a meibomian gland in the eyelid. The meibomian glands secrete oils that aid in lubricating the ocular surface. A chalazion should not be confused with a hordeolum which is an infectious, and often moderately painful, process. However, a chalazion may follow as an after-affect of a hordeolum. Most chalazia will resolve on their own but some require medical and/or surgical intervention. All new lumps and bumps should be evaluated as they can be an indication of skin cancer.
Conjunctivitis
Inflammation or infection of the conjunctiva, the transparent mucous membrane which lines the eyelids and covers the front part of the eyeball. Conjunctivitis may be caused by a bacterial or viral infection (“pink eye”) or an allergic reaction. Symptoms of conjunctivitis include: itching, burning, gritty feeling, excessive tearing, discharge, swollen eyelids, pink discoloration to the whites of the eyes and increased sensitivity to light. Viral and bacterial conjunctivitis are highly contagious. Treatment is aimed to increase comfort, reduce the length of time the patient has to suffer and to prevent the spread to other individuals.
Droopy Eyelids/Dermatochalasis
Droopy Eyelids – In Dermatochalasis, the eyelid skin becomes lax and falls in folds of redundancy over the eyelid margins. Patients often tell us they need to lift their eyelids so they can see. Blepharoplasty is surgery which removes fat, excess skin and muscle from the upper and/or lower lids. This surgery can be for cosmetic or functional reasons. When a patient has impaired vision due to droopy eyelids, specialized visual field testing and consultation in our office is performed to verify the medical necessity. We then work with eyelid surgical sub-specialists to facilitate care.
Diabetic Retinopathy
Diabetic retinopathy is progressive damage to the retina caused by diabetes. It is a serious sight-threatening complication of diabetes but may not have any symptoms in early stages. With diabetes, blood vessels throughout the body begin to leak blood and fluid. Patients with diabetic retinopathy are at increased risk for a retinal detachment. When our doctors look into your eyes with a medical microscope, they are evaluating the retina including the retinal blood vessels. Our Canon digital imaging system can be used to document retinal findings. Many patients are first diagnosed with diabetes based on findings from an eye exam. Patients with diabetes need to have their eyes examined, including dilation of the pupils, at least annually. The longer a patient has diabetes, the more likely they are to develop diabetic retinopathy. If adequate blood glucose control is not sufficient for controlling diabetic retinopathy, surgical options can be explored from a fellowship trained retinal sub-specialty ophthalmologist.
Our Canon digital imaging system can be used to document retinal findings (see the image below)

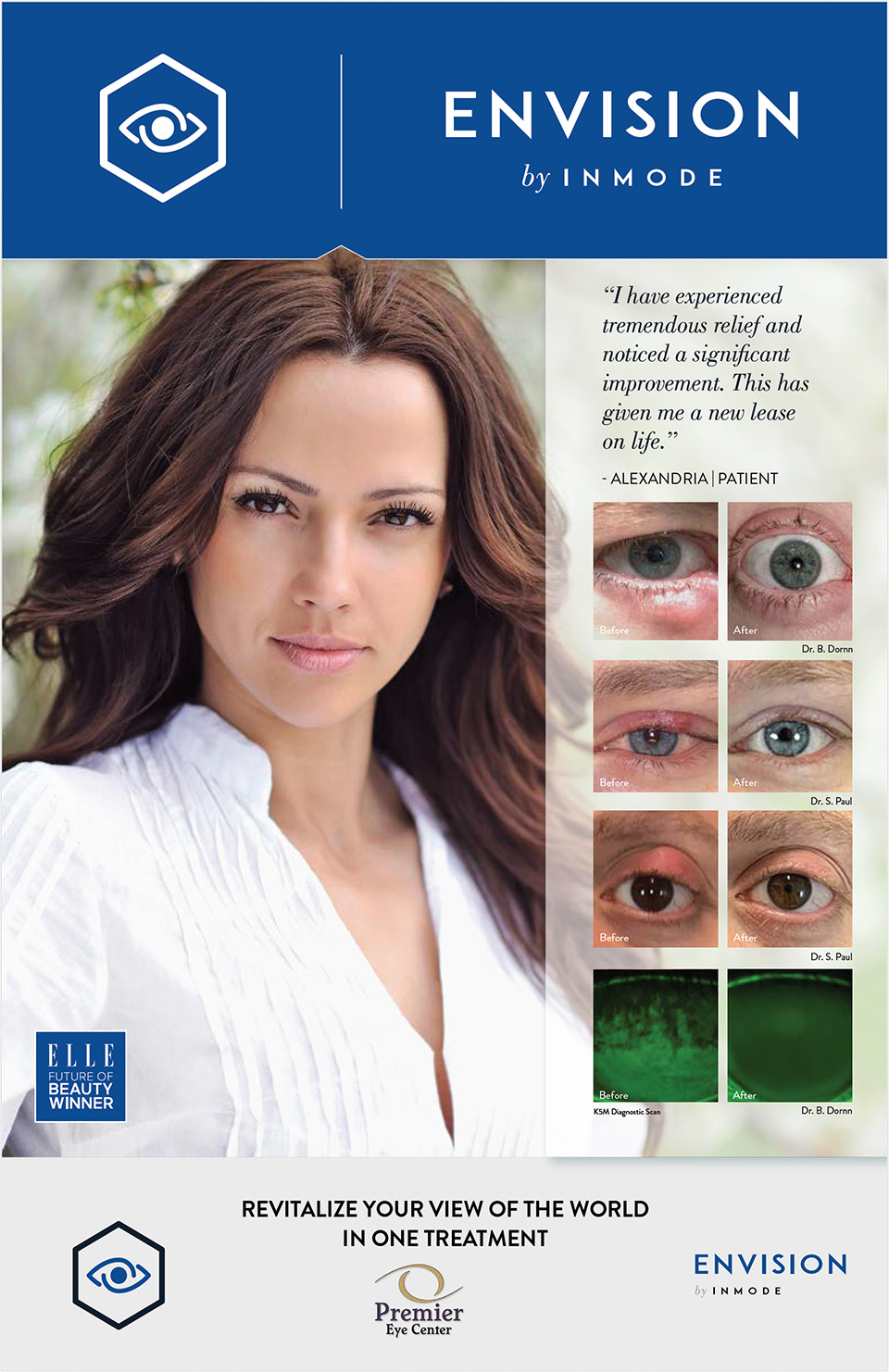
Dry Eye Syndrome
Dry Eye Syndrome is caused by insufficient lubrication for the eye. This can be caused by an inadequate volume of tears and/or poor quality of tears. Our doctors are experts in diagnosing and treating both types.
Patients with Dry Eye Syndrome may experience symptoms of burning, stinging, irritation, gritty, scratchy eyes, a feeling of something in the eyes, excess watering and/or blurred vision. Patients often marvel that their eyes can be watery and dry at the same time. The feedback loop between the eye and brain can get incorrect signals so the eye produces the wrong type of tears. Living in Prescott at mile-high elevation and very little humidity places many of our patients at risk of developing dry eyes. Many systemic medications can cause and/or exacerbate dry eyes. The most common offenders are medications for: blood pressure, allergies, depression and anxiety. It is usually not necessary to discontinue the medication but rather treat the dry eyes. Having dry eyes is not only painful and irritating but places the patient at risk of infection and scarring as well as making allergic conjunctivitis much worse. Treatment is tailored to each patient and may consist of over-the counter, prescription, surgical and natural remedies. More information about intracanalicular plugs. Blepharitis is often a significant contributor to dry eye disease.
We are excited to now offer BlephEX treatment to aid in the management of blepharitis. Click here to read more.

Flashes / Floaters
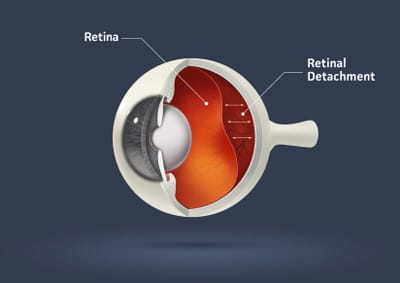
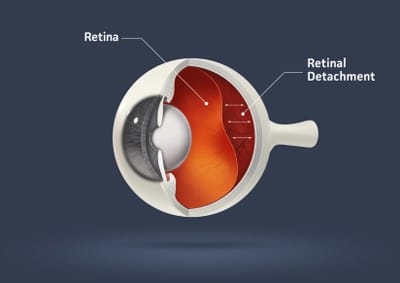
Floaters are small, semi-transparent or cloudy particles within the vitreous gel inside the eye. They can appear as specks, spots, threadlike strands or cobwebs of various shapes and sizes. Because they are located inside the eye, floaters move with the eye and seem to move away when you try to look at them. Floaters are most commonly associated with the breakdown of the vitreous gel as it becomes more watery. This is a part of the aging process. Floaters can also be signs of more serious problems including a retinal tear or detachment (see the image below). When the vitreous gel pulls on the retina, patients will notice flashes of light. The retina cannot say “ouch” but it can signal lights on or off. This traction can cause a retinal tear or detachment. All patients noticing flashes of light and/or new floaters should call our office for an urgent evaluation.
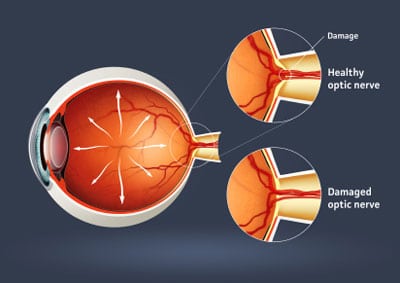
Glaucoma
Glaucoma is an eye condition causing damage to the optic nerve that can lead to blindness. The optic nerve is the cable which transmits signals from the retina to the brain. Early diagnosis and treatment are key to controlling glaucoma and saving sight. When caught early, glaucoma can usually be controlled. Glaucoma typically has no symptoms meaning it is up to an eye doctor to diagnose it rather than having a patient present with a complaint related to glaucoma. Glaucoma affects side vision leaving a patient with tunnel vision in late stages. Risk factors for glaucoma include: advancing age, family history of glaucoma, eye injury or surgery, African ancestry and elevated pressure within the eye. All of our comprehensive eye examinations include testing for glaucoma. If a patient is diagnosed as a glaucoma suspect (by our doctors or referred to us from outside doctors), Our skilled doctors will complete a glaucoma evaluation. Glaucoma was once thought to be due solely to high pressure inside the eye. We now know that many patients with normal intraocular pressure have glaucoma and need treatment. Treatment generally consists of medicated eyedrops.
Hordeolum or “stye”
Acute inflammation of a sebaceous gland in the margin of the eyelid, due to infection and usually resulting in the formation of pus. A hordeolum is a similar process to acne and may form a white head. All hordeolums should be evaluated to determine the proper course of action. Our doctors will help you determine what steps to take which may include: heat applied to site, drainage, and medical therapy consisting of drops and/or oral antibiotics.
Hyperopia (Farsightedness)
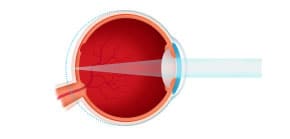
Vision condition in which distant objects are usually seen clearly but close ones do not come into proper focus. In this condition, the eye is too short and/or the cornea too flat so light is focused behind the retina.
(see the image below)
To correct hyperopia, eyeglasses or contact lenses are used to focus the light on the retina. Many young patients can manage small amounts of hyperopia by utilizing the accommodative (focusing) system inside the eye to focus the light on the retina. However, this can cause eye strain, fatigue, headaches, burning eyes or irritability and nervousness with prolonged work.
When presbyopia sets in, patients who were once able to cope with small amounts of hyperopia are no longer able to do so and need help with contacts and/or eyeglasses.
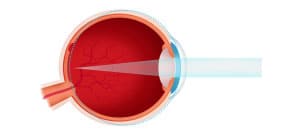
IOL
Short hand for “Intraocular Lens.” An IOL is placed into the eye following cataract surgery. (see the image below)
Keratoconus
A disorder that occurs when the normally round cornea becomes thin and irregular taking on a more conical shape. This abnormal shape causes light to be focused incorrectly and leads to distortion of vision. Each patient is different and symptoms vary from slight blurring and distortion of vision to legal blindness. In its early stages, keratoconus can be corrected with soft contact lenses and/or eyeglasses. As keratoconus advances and the cornea takes on a more irregular pattern, special rigid gas permeable (RGP) contact lenses will be required. An exciting advancement for our patients is the new SynergEyes contact lens combining the clarity of an RGP lens with the comfort of a soft contact lens. In rare cases surgery is necessary.
Macular Degeneration
The macula is the small area of the central retina that surrounds the fovea; this region provides our 20/20 vision. Age related macular degeneration (ARMD) is the leading cause of severe vision loss in adults over 50. There are two types of macular degeneration: dry and wet. Dry, or atrophic, macular degeneration is much more common than wet, or exudative. Symptoms of ARMD include: blurry central vision, distortion of vision (straight lines appearing wavy), loss of color vision and a dark or empty area appearing in the center of vision. Patients with advanced macular degeneration will never go “completely lights out” blind. Some side vision will eremain. Our doctors diagnose and monitor ARMD using a medical microscope and digital imaging system. There is no cure for dry macular degeneration but more and more studies are showing a link between proper nutrition and healthy function of the retina. Our doctors can help you determine an appropriate course of action and answer questions you may have about nutritional supplementation. For wet macular degeneration, injections into the eye can be performed by a retina specialist. All patients with ARMD, or who have family members with ARMD, should protect their eyes from the sun, stop smoking, eat a balanced diet low in fat and including dark leafy greens, and have their eyes evaluated at least annually.

Myopia (Nearsightedness)
Vision condition in which near objects are seen as clear and distance objects blurry. In this condition, the eye is too long and/or the cornea too steep so light is focused in front of the retina. To correct myopia, eyeglasses or contact lenses are used to focus the light on the retina. To determine the correct prescription, our eye doctors perform a refraction. As part of the testing, letters on a distance chart are identified. This test measures visual acuity, which is written as a fraction such as 20/40. The top number of the fraction is the standard distance at which testing is performed, twenty feet. The bottom number is the smallest letter size read. A person with 20/40 visual acuity would have to get within 20 feet to identify a letter that could be seen clearly at forty feet in a “normal” eye. Normal distance visual acuity is 20/20, although many people have 20/15 (better) vision.
The exact causes of myopia are unknown but there are certainly hereditary and environmental components. If one or both parents is nearsighted, there is an increased chance their children will be as well. Individuals who spend a considerable amount of time reading, using the computer, or other intense near work may be more likely to develop myopia. Patients who are very myopic (strong prescription) are at an increased risk of retinal tears and detachments due to lengthening of the eyeball. Myopia can also be a sign of inadequate blood glucose control and one of the first signals of diabetes. Some forms of cataracts will cause a patient to develop myopia and/or become more myopic requiring a stronger prescription.
Pinguecula
An abnormal growth of tissue on the conjunctiva, the clear membrane covering the white of the eye. Most commonly due to prolonged irritation: wind, dust and UV. It is best to treat pingueculae with aggressive prevention by limiting exposure to irritants. Our optical staff can help you select the best sunglasses to keep irritants at bay. Pingueculae act as speed bumps each time you blink. Adequate lubrication is a must and Dr. Sullivan and his team often recommend intracanalicular plugs to ensure adequate lubrication is present. Pinguecula may become red, itchy and irritated necessitating medical therapy. Pinguecula are almost never operated on. More information about intracanalicular plugs.
Presbyopia
Vision condition in which the crystalline lens loses its flexibility thus weakening the accommodative (focusing) system and making it difficult to focus on close objects. This usually takes place over the course of years although many patients describe it as happening “overnight.” Presbyopia usually becomes noticeable in the late 30s to early 40s. It is a normal part of the aging process, is not a disease, and cannot be prevented. Signs of presbyopia include blurred vision at normal reading distance, eye fatigue and headaches with near work and a tendency to hold reading material further away. Many patients tell us their arms are too short. The good news is we have many options to help compensate for presbyopia. These include: Progressive Addition Lenses (PALs), reading glasses, bifocals, trifocals, and even contact lenses.
Pterygium
A triangular fold of growing tissue which extends from the conjunctiva over the cornea. Most commonly due to prolonged irritation: wind, dust and UV. It is best to treat pterygium with aggressive prevention by limiting exposure to irritants. Our optical staff can help you select the best sunglasses to keep irritants at bay. Pterygia act as speed bumps each time you blink. Adequate lubrication is a must and often recommend intracanalicular plugs to ensure adequate lubrication is present. Pterygia may become red, itchy and irritated necessitating medical therapy. Rarely a pterygium becomes large enough to cover the pupil and obscure vision warranting surgical intervention. More information about intracanalicular plugs.
Retinal Detachment
A tear, or separation, of the retina from the underlying tissue. A retinal detachment may give symptoms of flashes/floaters or may be asymptomatic. A retinal detachment is an ocular urgency and should be addressed as soon as possible. (see the image below)
Strabismus
Also known as an eye-turn. Strabismus is when one or both eyes do not point where they are supposed to. The eyes can turn in, out, up or down. This is usually caused by a muscle imbalance but can also be due to uncorrected refractive error, diabetes, hypertension and neurological issues. Strabismus can lead to amblyopia. Treatment is tailored to each individual and may consist of: eye exercises, special eyeglasses with or without prism, contact lenses or surgery.
Stye
see Hordeolum